The first person cured of HIV.
- Maya Witowska
- Jan 25, 2021
- 6 min read
What can we learn from Timothy Ray Brown – the first person cured of the Human Immunodeficiency Virus (HIV)?
According to the UNAIDS website, there were as many as 38 million cases of HIV/AIDS worldwide. [1] Together with tuberculosis and malaria, HIV is one of the “big three”; infections with extremely high incidence that don’t have a functioning cure. There is, however, a person that was cured of HIV – Timothy Ray Brown. Though it was replicated in the London Patient, the treatment isn’t actually one that can be administered to every HIV-positive individual. It does offer the basis for new therapy approaches and expands existing research possibilities in the search for the ever-evasive HIV “cure”.
Who was Timothy Ray Brown?

Timothy Ray Brown in 2019. Photographed for an article in The New York Times. [4]
Timothy Ray Brown was 54 years old when he died on the 29th September 2020. In 2006, he was diagnosed with Acute Myeloid Leukemia (AML) – a cancer with a 5-year survival rate of 25%. [2] So how did Timothy live for another 14 years with an AML diagnosis? He was treated with a haemapoietic stem cell transplants (HSCT); a procedure that replaces your defective cells in the bone marrow with those able to produce cells for your blood. [3] However, Timothy wasn’t an ordinary patient. He was the Berlin Patient; the first person to be cured of HIV. The same transplant that was used to treat his leukemia cured him of the Acquired Immunodeficiency Syndrome (AIDS). This article will focus on the significance of this phenomenon on the past and current state of HIV pandemic and why the HSCT isn’t a final solution to curing the virus.
The Berlin Patient
Timothy was studying at a Berlin university when he received an HIV diagnosis in 1995. He started taking Zidovudine (AZT)- a drug approved just 8 years before. He was later prescribed more medicines to treat the virus, as the pathogen could become resistant or find new ways to infect the cells of the host. The therapy seemed to be working, with Timothy feeling generally well for the next 10 years. However, a decade later, he started feeling increasingly weak and was diagnosed with anaemia (caused low red blood cells or low haemoglobin) that turned out to be a symptom of leukemic cancer. [4] He was sent to a Charite hospital in Berlin, where he began chemotherapy under the supervision of Dr. Gero Huetter. Those treatments caused him to catch pneumonia and go into a coma, what prompted his physician to think of another therapeutic possibilities. His solution was to perform an HSCT, but using cells from a donor that had a mutation that made him partly resistant to HIV to “to kill birds with one stone”. The risky procedure went well; not only was Timothy cancer-free, he also didn’t have any HIV particles in his blood when it was measured 3 months after the operation. Though the AML came back in 2008, which prompted a second HSCT that had severe side effects, Timothy Ray Brown remained free of HIV until his death. [5]
The mutation
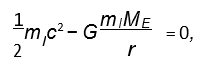
The Human Immunodeficiency Virus (HIV) only infects cells that have specific receptors which allow it to go inside host cells and replicate. The main receptor is called CD4, and is mostly found on lymphocytes that help initiate immune responses to fight pathogens. Each of these CD4+ T cells have one of two co-receptors that HIV also needs for entry: CCR5 or CXCR4. [6] The mutation that “cured” Timothy of the virus is called CCR5 Delta 32. [7] This means that the cells he received had no CCR5 receptor. HIV needs both the main receptor (CD4+) and a co-receptor (CCR5 or CXCR4) to infect the host. If even one of them is missing, it will likely not be able to replicate and die. Therefore, when Timothy received the “HIV-resistant” cells during HSCT, HIV could no longer infect them and the remaining virus was destroyed by Timothy’s immune system, curing him of the disease.
Why CCR5 delta 32 isn’t an effective anti-HIV therapeutic?
As mentioned above, HIV can use two different co-receptors to infect lymphocytes. The transplantation of cells without the CCR5 cured Timothy Brown, because this is the receptor the virus uses most often. However, HIV can be specific for CXCR4, or mutate to be able to use it, instead of CCR5. This means that HSCT of cells lacking CCR5 doesn’t necessarily mean that the virus won’t be able to infect the new cells.
It’s important to remember that Timothy received the transplant only because he was suffering from AML; HSCT isn’t a commonly done procedure for a number of important reasons. Most importantly, it’s an incredibly risky procedure with a survival rate of 50% when Timothy Brown received the transplant. Even today there is only a 50% of success with every HSCT. [8] Not only is there a risk of relapse, but there is a possibility of a range of mild to severe side effects; after the second HSCT Timothy went nearly blind and almost paralyzed.
The haemapoietic stem cell transplant isn’t an effective solution not only from the biological, but also purely logistical point of view. As with any transplantation procedure, the cells of the donor need to match the recipient so they won’t be rejected. In this case, cell matching is even harder, as donor cells must also contain the “HIV-resistant” mutation, which rarely appears in the population (between 16.4% and 0% depending on the country). [9] Finally, the procedure requires the patient to stay in a controlled environment for an extensive period of time in addition to high financial cost either for the patient or the institution conducting operation.
The past, present, and future of HIV/AIDS therapy
When the HIV pandemic first started to become noticeable in the 1980s, AIDS diagnosis was a death sentence – life expectancy for affected patients was no more than one year. The antiretroviral therapy (ART) revolutionised HIV treatment when it was first introduced in the mid 1990s. [10] Though this approach demands a strict life-time routine of drug taking, it also prevents symptoms, or even stops the progression to AIDS, resulting in a life expectancy close to that of a healthy individual.
In 2019, The London patient was the second person cured of HIV. He underwent the same treatment as Timothy Ray Brown, as he suffered from a Hodgkin lymphoma that made him eligible for the transplant. [11] Though this approach remains a non-feasible treatment option for the majority of HIV patients, the two cases provided significant insight into the research on the elusive HIV “cure”. For example, a possibility to use gene editing for a less invasive way to introduce CCR5-lacking cells into patients, or utilizing one of the co-receptors as a vaccine target. Before any of that can be achieved, the current multidrug regimen – ART, is an effective way to lower the viral load so that any HIV-positive person is able to lead a relatively normal life.
Author:
Maja Witowska
Keble College
MSc Integrated Immunology
References
1. HIV.gov. 2020. Global Statistics. [online] Available at: <https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics> [Accessed 17 November 2020].
2. Cancer Research UK. 2020. Acute Myeloid Leukaemia (AML) Survival Statistics. [online] Available at: <https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/leukaemia-aml/survival> [Accessed 17 November 2020].
3. H, F. and GG, H., 2020. Hematopoietic Stem Cells: Potential New Applications For Translational Medicine. [online] PubMed. Available at: <https://pubmed.ncbi.nlm.nih.gov/25157450/> [Accessed 17 November 2020].
4. Nytimes.com. 2020. Timothy Ray Brown, First Patient Cured Of H.I.V., Dies At 54. [online] Available at: <https://www.nytimes.com/2020/09/30/health/timothy-ray-brown-first-patient-cured-of-hiv-dies-at-54.html> [Accessed 17 November 2020].
5. Who.int. 2020. Anaemia. [online] Available at: <https://www.who.int/health-topics/anaemia#tab=tab_1> [Accessed 17 November 2020].
6. Brown, T., 2015. I Am the Berlin Patient: A Personal Reflection. AIDS Research and Human Retroviruses, 31(1), pp.2-3.
7. Alkhatib, G., 2009. The biology of CCR5 and CXCR4. Current Opinion in HIV and AIDS, 4(2), pp.96-103.
8. Watts, G., 2020. Timothy Ray Brown. The Lancet, 396(10259), p.1327.
9. Henig, I. and Zuckerman, T., 2014. Hematopoietic Stem Cell Transplantation—50 Years of Evolution and Future Perspectives. Rambam Maimonides Medical Journal, 5(4), p.e0028.
10. Solloch, U., Lang, K., Lange, V., Böhme, I., Schmidt, A. and Sauter, J., 2017. Frequencies of gene variant CCR5-Δ32 in 87 countries based on next-generation sequencing of 1.3 million individuals sampled from 3 national DKMS donor centers. Human Immunology, 78(11-12), pp.710-717.
11. Niaid.nih.gov. 2020. Antiretroviral Drug Discovery And Development. [online] Available at: <https://www.niaid.nih.gov/diseases-conditions/antiretroviral-drug-development> [Accessed 17 November 2020].
12. Virology.ws. 2020. The London Patient. [online] Available at: <https://www.virology.ws/2019/03/13/the-london-patient/> [Accessed 17 November 2020].


Comments